Everything you wanted to know and were afraid to ask about Demodex
It is almost impossible to pick up a clinical journal or go to a conference, lately, without stumbling upon the topic
of Demodex. Although the significance of this parasite for humans was descri bed as early as the 1960s,1-3 its
clinical relevance attracted limited attention. The incorporation of both diagnostic and therapeutic informatio n
has catapulted this organism to be the buzzword of the day in t he realm of ocular surface health. Most clinicians
vaguely remember, if at all, a brief description of Demodex in their ocular health course on lid disease. Little was
known about the organism, except that it was often described as ‘found universally’ in older adults.4 However, its
association with other ocular anomalies were unknown so consequ ently it fell off the differential diagnosis radar
as a potential cause of anterior segment afflictions. This editorial offers an overview of the current knowledge on
Demodex and its relevance to clinical practice.
What is Demodex?
Although several species of Demodex exist, only two inhabit humans, namely Demodex folliculorum and Demodex brevis.2, 5-12 This ectoparasite (living outside the human body) is the most c ommon organism found on the human body and its presence increases with age. D. folliculorum, the larger of the two species (0.3-0.4mm), has an affinity for hair follicles including eyelashes, eyebrows , nose and ear hair, scalp, chest hair, underarms, etc. and is typically found in groups of mites. Alternatively, the shorter species, D. brevis (0.2-0.3mm), has a preference for sebaceous glands, including those on the face an d the meibomian glands and tends to live on its own. The word Demodex originates from the Greek word ‘demos’ meaning ‘fat’ and ‘dex’ meaning ‘worm’.2
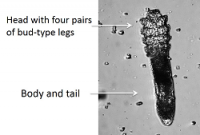
The life cycle of Demodex varies between 14 to 18 days, going through dif ferent stages starting with the egg to
larval stage to adult mite.11-13 The adult mite has four bud-type legs on either side of its hea d, and has a head to
body ratio11 of 1:2 for the D. folliculorum and a 1:1 for D. brevis.
Female mites can lay as many as 10-12 eggs at a time, consequen tly leading to overpopulation of the infected
area if left unmanaged. Prevalence of Demodex infestation increases with age, with a reported 84% in people >60
and 100% of patients >70 years of age. 1,10 Direct contact is needed to transfer mites from one person to another,
most probably through common household items such as linen, tow els and toiletries.10,14 Contact lens wearers,15
those afflicted with acne rosacea,16-19 immuno-compromised patients,20-23 patients with blepharitis24-26 or history of
chalazia27-29 have been reported to harbour greater numbers of Demodex.
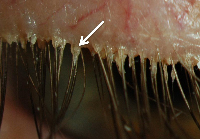
The existence of the mite outside the human body is limited, al though the exact timing is unknown.11 The
Demodex mite avoids light and buries itself head first in the follicles or glands, with only the tail visible at the
opening of the lash follicle.2,10 The D. folliculorum mite burrows down the eyelash follicle to lay its eggs and
ingests the gland lining using its sharp mouth, resulting in fo llicular distension and trichiasis (misdirected lashes).
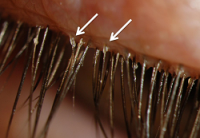
Debris generated from the mites accumulates at the root of the lashes and is clinically observed as a gelatinous
cylindrical ‘sleeve’ or cylindrical dandruff (CD) at the base of the eyelash, which are pathognomonic for mite
infestation.30
This debris can be differentiated from other debris on the lashes, caused by make-up and other causative factors of anterior blepharitis (e.g. Staphylococcus aureus). One key i ndicator is that the cylindrical dandruff remains at the root of the lashes and is independent of lash growth. Co ntrary to the flaky yellow “collarettes” typical of blepharitis secondary to Staphylococcal aureus infection, which are found at any point on the lash as it elongates, the cylindrical dandruff associated with Demodex remains at the base of the lash.
Demodex mites have also been reported to act as vectors for bacteria ( staphylococci and streptococci), either by carrying them on their body or within their gut ( bacillus oleronius). Either way, the mite, its waste and cytoskeleton may all be contributory factors in generating an inflammatory or even an immune response on the ocular surface.11,19,27,31
Clinical evaluation of Demodex folliculorum
Symptoms of Demodex infestation include ocular discomfort, itchiness, burning, for eign body sensation, blurry vision and dryness.10,32 One of the key symptoms in ocular demodicosis is itching, 33 especially along the lid margin. To date, there is no convincing evidence which correlates the mi nimum number of mites required to induce symptoms.11,34 Some Demodex-positive patients may even be asymptomatic,9 further confounding the true prevalence of Demodex, as these patients are less likely to present for examination.
Ocular signs include the pathognomonic cylindrical dandruff at the base of the lashes, trichiasis (misdirected lashes), madarosis (loss of lashes), telangiectasia and ocular hyperemia. Strong evidence of comorbidities has been reported, including meibomian gland dysfunction,24-26 recurrent chalazia27-29 and acne rosacea.16-19, 31
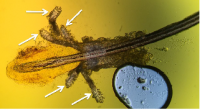
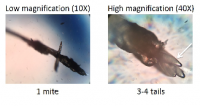
To date, confirmation of diagnosis involves epilation of several sample lashes with cylindrical dandruff, which are then transferred to a microscopic slide so that the lashes and mites can be observed ex-vivo under a light microscope.10-11
Confocal microscopy remains the only technique, to date, to vie w the mites in vivo, but this technology is likely to be restricted to an academic or research setting. Sup plementary clinical observations have been proposed, including pinching the affected lash with tweezers and rotating it while observing, unde r high slit lamp magnification, the tails of the mite emerge from the follicle. 36 Emerging technologies that are helpful in viewing Demodex include the BlephCam (Scope Ophthalmics, UK),37 a portable illuminated digital camera that magnifies the lid margin to enhance observation. The BlephCam offers an alternative to view the lid margin and educate patients if anterior segment imaging is not available.
A proposed severity scale for ocular Demodex infestation, or dem odicosis, is dependent on the number of lashes with cylindrical dandruff.38 Severity can be divided into mild (<5 lashes with cylindrical dandruff), moderate (5-9 lashes with cylindrical dandruff) and severe (>10 lashes have cylindrical dandruff); however, this scale is not yet widely utilized.
Management of Demodex infestation
The emphasis of therapy hinges on reducing the numbers of mites and alleviating symptoms such as itching. As with any therapy, patient education is key, to explain the nature of the problem and the life cycle of th e parasite so that compliance is maintained for the prescribed period of t ime. Effective treatments against Demodex include pilocarpine gel,39 oral ivermectin for ocular and skin demodicosis 40-41 and tea tree oil.42-45 Tea tree oil is derived from the leaves of Melaleuca alternifolia, a tree native to Australia, which possesses anti-microbial properties.42 In its pure form, it is extremely harsh to the skin, hence pati ent education is crucial in avoiding severe ocular irritation. Consequently, commercial formulations contain diluted tea tree oil, althoug h the degree of dilution is not always divulged. Tea tree oil has been found to be toxic to the mites and assist in reducing mite counts by promoting their migration out of the follicles. They can then be removed by lid scrubs. 43-45
Further research into tea tree oil has indicated that the activ e ingredient that Demodex is most sensitive to is terpinen-4-ol (T4O).46 The only commercially available lid scrub with T4O is Cliradex® (Biotissue, USA), which remains the treatment of choice for many sufferers.11 The recommended regimen involves cleaning along the lash line twice a day (bid) for three weeks, followed by a nightly t reatment for another three weeks, to coincide with the lifecycle of the mite and the eggs that will subsequently h atch. It is recommended that clinicians demonstrate the use of Cliradex® with patients, as it is associated with a cooling/burning sensation similar to that produced by menthol. Other lid scrubs intended for at home use and conta ining varying amounts of diluted tea tree oil formulations include: SteriLid (Theratears/Akorn),48 Ocusoft Lid Scrub PLUS (Ocusoft),49 I-lid’n Lash PLUS (I-med pharma)50 and BlephaDex (Macular Health),51 but studies on these products have yet to be published.
Products designed for in-office use have also emerged, such as I -lid’n Lash PRO (I-med pharma),50 with 20% tea tree oil, and Oust™ Demodex® Swabstix™ (Ocusoft), 52 with a combination of tea tree oil, sea buckthorn and coconut oil, however their efficacy have not yet been reported i n the literature. Patient instruction is key in using these products, as the increased tea tree oil concentration is harsher to the skin and ocular surface and may necessitate topical anesthesia prior to use. Mechanical cleanin g along the lash line using a novel instrument, BlephEx (Rysurg),53 has also been shown to alleviate symptoms of anterior blephari tis and dislodge debris via a rotating disposable medical sponge tip.
Patients can also contribute to limiting re-infestation by chan ging linen and towels more often, discarding eye makeup such as mascara, using tea tree oil-based shampoo for th eir hair and having close family members checked.
Demodex infestation has been shown to affect ocular comfort,10,32 play a role in skin (acne rosacea) and ocular (blepharitis, chalazia) afflictions9 and potentially lead to discontinuation of contact lens wear.14 These should all be strong motivators for clinicians to take a proactive role in identifying Demodex and advocating for a healthy lid margin.
REFERENCES
1. Post CF, Juhlin E. Demodex folliculorum blepharitis. Arch Dermatol 1963;88: 298-302. 2. Coston TO. Demodex folliculorum blepharitis. Trans Am Ophthalmol Soc 1967;65: 361-92 3. Akbulatova LK. The pathogenic role of Demodex mite and the clinical form of de modicosis in man. Vestnik Dermatologii i venerologii 1963;40: 57-61 4. Catania LJ. Demodicosis. In ed. Primary Care of the Anterior Segment, 2nd edition. 1995; Appleton & Lange; Norwalk, Connecticut. 5. Edmondson II W, Christenson MT. Lid Parasites. In: Clinical Optometric Pharmacology and Therapeutics (Onefrey B, editor., Lippincott-Raven, Philadelphia: 1992. 6. Lacey N, Kavanagh K, Tseng SC. Under the lash: Demodex mites in human diseases. Biochem (Lond). 2009;31(4): 2-6. 7. Nutting WB. Hair follicle mites (Acari: Demodicidae) of man. Int J Dermatol 1976;15(2): 79-98. 8. English FP, Nuttin WB. Demodicosis of ophthalmic concern. Am J Ophthalmol 1981;91: 362-372. 9. Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol 2010 10(5): 505-10. 10. Hom MM, Mastrota KM, Schachter SE. Demodex. Optom Vis Sci 2013 90(7): e198-205. 11. Cheng AMS, Sheba H, Tseng SCG. Recent advances on ocular Demodex infestation. Curr Opin Ophthalmol 2015;26: 295-300. 12. Rufli T, Mumcuoglu Y. The hair follicle mites Demodex folliculorum and Demodex brevis : Biology and medical importance. A review. Dermatologica 1981;162: 1–11. 13. Rather PA, Hassan I. Human Demodex Mite: The versatile mite of dermatological importance. Indian J Dermatol 2014;59(1): 60–66. 14. Tarkowski W, Moneta-Wielgos J, Mlocicki D. Demodex sp. As a potential cause of the abandonment of soft contact lenses by their existing users. Biomed Res Int 2015 Epub ahead of print (http://www.ncbi.nlm.nih.gov/pubmed/26290865). 15. Jalbert I, Rejab S. Increased numbers of Demodex in contact len s wearers. Optom Vis Sci 2015;92(6): 671-8. 16. Forton F, Seys B. Density of Demodex folliculorum in rosacea: a case co ntrol study using standardized skin-surface biopsy. Br J Dermatol 1993;128: 6509. 17. Erbagci Z, Ozgostasi O. The significance of Demodex folliculorum density in rosacea. Int J Dermatol 1998;37: 421-5. 18. Lacey N, Delaney S, Kavanagh K, et al. Mite-related bacterial a ntigens stimulate inflammatory cells in rosacea. Br J Dermatol 2007;157: 474-81. 19. Li J, O’Reilly N, Sheba H et al. Correlation between serum immu ne-reactivity to Demodex-associated Bacillus proteins in patients with facial rosacea. Ophthalmology 2010;117: 870-7. 20. Holmes RB, Martins C, Horm T. The histopathology of folliculitis in HIV-infected patients. J Butan Pathol 2002;29: 93-5. 21. Aydingoz IE, Dervent B. Demodex folliculorum in renal transplant patients revisited. Dermatology 2001;203: 272-3. 22. Erbagci Z, Erbaci I, Erkilic S. High incidence of demodicidosis in eyelid cell carcinomas. Int J Dermatol 2003;42: 567-71. 23. Castanet J, Monpoux F, Mariani R et al. Demodicidosis in an immunodeficient child. Pediatr Dermatol 1997;14: 219-220. 24. De Venecia AB, Siong RLB. Demodex sp. Infestation in anterior blepharitis, meibomian gland dysfunction, and mixed blepharitis. Philippine J Ophthalmol 2011;36: 15-22. 25. Zhao YE, Wu LP, Xu JR. Association of blepharitis with Demodex: A meta-analysis. Ophthalmic Epidemiology 2012;19(2): 95-102. 26. Bhandari V, Reddy JK. Blepharitis: Always remember Demodex. Middle East Afr J Ophthalmol 2014;21(4): 317-320. 27. Liang L, Ding X, Tseng SC. High prevalence of Demodex brevis infestation in chala zia. Am J Ophthalmol 2014;157: 342-8. 28. Schear MJ, Milman T, Steiner T, et al. The association of Demodex with chalazia: A histopathologic study of the eyelid. Ophthal Plast Reconstr Surg 2015; Epub ahead of print (http://www.ncbi.nlm.nih.gov/pubmed/26108058). 29. Tarkowski W, Owczynska M, Blaszczyk-Tyszka A, et al. Demodex mites as potential etological factor in chala zion-a study in Poland. Acta Parasitol 2015;60(4)777-83 Epub ahead of print (http://www.ncbi.nlm.nih.gov/pubmed/26408604). 30. Gao YY, Di Pascuale MA, Li W et al. High prevalence of Demodex in eye lashes with cylindrical dandruff. Invest Opthalmol Vis Sci 2005;46: 3089-94. 31. O’Reilly N, Menezes N, Kavanagh K. Positive correlation between serum immuno-reactivity to Demodex-associated Bacillus proteins and erythematotelangiectic rosacea. Br J Dermatol 2012;167: 1032-6. 32. Lee SH, Chun YS, Kim JH, et al. The relationship between Demodex and ocular discomfort. Invest Ophthalmol Vis Sci 2010;51: 2906-11. 33. Gao YY, Xu DL, Huang l J, Wang R, et al. Treatment of ocular itching associated with ocular demodicosis b y 5% tea tree oil ointment. Cornea 2012;31(1): 14-7. 34. Wesolowska M, Knysz B, Reich A, et al. Prevalence of Demodex spp, in eyelash follicles in di fferent populations. Arch Med Sci 2014;10: 319-24. 35. Randon M, LiangH, El HM et al. In vivo confocal microscopy as a novel and reliable tool for the diagnosis of Demodex eyelid infestation. Br J Ophthalmol 2015;99: 336-41. 36. Mastrota KM. Method to identify Demodex in the eyelash follicle without epilation. Optom Vis Sci 2013;90(6): e172-4. 37. Blephcam, Scope Ophthalmics. URL http://www.blephexlids.co.uk/blephcam%E2%84%A2 (Accessed Oct 28, 2015) 38. Schachter S. A different approach to treating demodex blepharitis. Optom Times. 2014 Jan 3. URL http://optometrytimes. modernmedicine.com/optometrytimes/content/tags/blephex/different-approach-treating-demodex-blepharitis. (Accessed Oct 28, 2015). 39. Fulk GW, Murphy B, Robins MD. Pilocarpine gel for the treatment of dem odicosis-A case series. Optom Vis Sci 1996;73: 742-5. 40. Salem DAB, El-Shazly A, Nabih N et al. Evaluation of the efficacy of oral ivermectin in comparison with ivermectin-metronidazole combined therapy in the treatment of ocular and skin lesions of Demodex folliculorum. Int J Infectious Diseases 2013;17: e343-7. 41. Holzchuh FG, Hida RY, Moscovici BK, et al. Clinical treatment of ocular demodex fol liculorum by systemic ivermectin. Am J Ophthalmol 2011;151: 1030-4. 42. Carson CF, Hammer KA, Riley TV. Melaleuca alternifolia (Tea Tree) oil: a review of antimicrobial and other medicinal propert ies. Clin Microbiol Rev 2006;19(1): 50-62. 43. Gao YY, Di Pascuale MA, Li W, et al. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br J Ophthalmol 2005;89(11): 1468-73. 44. Gao YY, Di Pascuale MA, Elizondo A, et al. Clinical treatment of ocular demodecosis by lid scrub with tea tree oil. Cornea. 2007;26(2): 136-43. 45. Koo H, Kim TH, Kim KW et al. Ocular surface discomfort and Demodex: ef fect of tea tree oil eyelid scrub in Demodex blepharitis. K J Med Sci 2012;27:1574-9. 46. Tighe S, Gao YY, Tseng SCG. Terpinen-4-ol is the most active ingredient of tea tree oil to k ill demodex mites. Translational Vis Sci Tech 2013;2: 1-8. 47. Cliradex. URL http://www.cliradex.com/ (Accessed Oct 28, 2015) 48. Sterilid (Theralid in Canada). URL http://www.theratears.com/sterilid/ (Accessed Oct 28, 2015). 49. Ocusoft Lid scrub PLUS. Ocusoft. URL http://www.ocusoft.com/ocusoft-lid-scrub-plus-pre-moistened-pads-30ctn (Accessed Oct 28, 2015). 50. I-lid’n Lash PLUS/PRO. I-MED Pharma Inc. URL http://imedpharma.com/ocular-hygiene (Accessed Oct 28, 2015). 51. BlephaDex. Macular Health. URL https://www.macularhealth.com/product/blephadex-eyelid-wipes. (Accessed Oct 28, 2015). 52. Oust Demodex Swabstix (Ocusoft) URL http://ocusoft.com/oust-demodex-swabstix-12box (Accessed Oct 28, 2015). 53. BlephEx. RySurg, LLC. URL http://www.rysurg.com (Accessed Oct 28, 2015).