Contents |
Blepharitis: Making Matters Worse
Introduction and Overview
Blepharitis, also known as meibomian gland dysfunction (MGD), is the term used for a family of eyelid margin disorders that cause symptoms such as redness, swelling, itching or burning, dryness, crusty lids, grittiness, and even eventual loss of eyelashes. If the lashes grow back, sometimes they no longer have pigment or they grow in the wrong direction, back towards the eye, which can cause a secondary irritation to the ocular tissues.
Causes can include an underlying bacterial infection, skin conditions like psoriasis, dandruff, or rosacea, environmental irritants like chemical fumes, smoke, or smog, or an infestation of the Demodex mite in the follicles of the eyelashes or eyebrow.
Blepharitis (pronounced “bleff-uh-right-iss”) rarely causes long-term vision loss but it can complicate cases of dry eye or infection. It can be acute, with a sudden onset, but it can also easily become chronic, unless the cause is eliminated or treated.
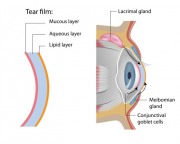
It helps to understand that the natural tears are composed of three main layers, each of which helps in keeping the eye lubricated. About 90% of the tears are made of what most people would call salt water; the other 10% keeps the tears in place on the surface of the eye and keeps them from evaporating too quickly. Tear quality as well as quantity is necessary.
When a meibomian gland becomes inflamed and/or infected, the result is called a stye, a chalazion or meibomianitis. These are acute and painful gland impactions, caused by the gland openings being blocked by bacterial debris. (Figure 1 shows the normal layers of the tear film on the left. The meibomian glands are located within the eyelids, both upper and lower.)
Untreated, blepharitis becomes chronic and can lead to meibomian gland stasis, which is the loss of function of one or more meibomian glands. Stasis is the loss of function of the gland, and results when the duct openings are clogged and the normal secretions cannot pass from the gland into the tears.
Blepharitis can adversely affect the outcome of cataract or refractive surgery, so patients considering either of these common surgeries must first have any existing blepharitis controlled as much as possible.
Many times, patients with blepharitis also experience symptoms of dry eye; if artificial tears or lubricants are being used, it is best to use unpreserved versions if possible, because the preservatives can themselves cause reactions.
Signs and Symptoms
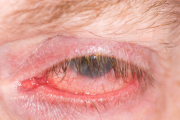
Eyelids that are red, especially around the eyelash line, swollen, itchy and crusty all are signs of blepharitis, as well as grittiness or the feeling of foreign bodies in the eye. The symptoms may be mild or more severe. Untreated, it can progress to involve the conjunctiva, the clear skin that covers the white of the eye and lines the insides of the eyelids, to become a condition known as blepharoconjunctivitis.
(Figure 2 shows how blepharitis can affect not only the eyelids, but can spread to the conjunctiva and become chronic. Note the sparse eyelashes.)
In the eyecare practitioner’s office, the eye can be evaluated for dryness using testing strips placed in the lower lids, staining of the tear film with dye that can be seen using the slit lamp, and expression of the materials from the meibomian glands can all be helpful.
Demodex Mites
Recently, more eyecare practitioners are becoming aware that blepharitis is often caused by the Demodex mite, which lives at the base of the eyelash hair follicles and sometimes in the hair follicles of the eyebrows or other areas of the face.
It is estimated that almost 85% of the population at age 60 have Demodex infestation, and by age 70, that percentage rises to almost 100%. The mites are also found in young adults, so it is not just significant for older patients, but must be considered as the possible cause of most cases of blepharitis.
Interestingly, Demodex mites have been increasingly associated with other skin disorders such as rosacea. Treating rosacea patients for Demodex not only makes their eyes more comfortable, but if the blepharitis is treated with both topical and systemic medications, most of the time their rosacea improves, too.
The main symptoms of Demodex infestation include itching or burning, foreign body sensation, redness of the lid margin, and blurred vision. With Demodex, the eyecare practitioner will see a cylindrical-shaped crustiness around the bases of the lashes. If the lashes are sampled, it is usually possible to see the mites under a light microscope.
Demodex may not always bother all people who have it. Some patients are asymptomatic, but an infestation can get out of control, in a similar way to how staph bacteria are usually present on most people’s skin.
Treatment
Hygiene is very important, as this clears away any debris that might be present. Warm compresses and lid massage, as well as lid scrubs are helpful to quiet the entire area. Warmth helps the meibomian glands function better, as it will make material clogging the ducts softer and easier to remove.
If there is an associated infection, antibiotics, either in the form of eyedrops or oral medication, may be added.
A useful tool for eyecare practitioners in the office is periodic treatment with the BlephEx, a small, handheld tool that helps to effectively remove debris from the lid margins, as well as to remove some of the clogging from the gland ducts. This is a rotating scrubber topped by a disposable sponge tip that can be used first in one direction, and then reversed so the lash follicles and gland ducts are cleaned from both directions. Each lid is cleaned thoroughly, then the tip is replaced for the other eye. The makers of the BlephEx tool recommend retreatment every four to six months, depending on the severity of the condition.
For Demodex mites, the only really effective treatment in the past has been tea tree oil, which does kill the mites and interrupts their life cycle. Recently, a new product has come on the market which uses the active ingredients in tea tree oil in a less-irritating form, called Cliradex.
Some practitioners advise a regimen of whole-body hygiene, including using regular shampoo or soap, as mites can easily travel from one area to another. Washing bedding weekly and drying in a hot dryer is an effective means of removing that possible source, as heat will kill the mites.
There are various lid scrub preparations on the market and available over-the- counter that are helpful if the blepharitis is not being caused by Demodex. These, along with warm compresses and lid massage will help unclog blocked ducts and help the meibomian glands to function.
If it is determined that blepharitis is being caused by Demodex, tea tree oil or Cliradex can be used as an effective way to interrupt the short life span and mating cycle of the mites.
Cliradex is a combination of natural ingredients to clean the area around the eye, including the lashes and the skin. It is a two-step system that includes an eyelash/lid scrub and a cleansing skin cream. The scrub gets the mites out from deeper in the skin and can be directly killed, while the cream prevents them from mating.
New methods of treating blepharitis are becoming available as more research is being done using radio frequency energy to produce heat. In the meantime, maintaining good hygiene is a key factor, as Demodex will return if given the chance.
If the patient with blepharitis is a contact lens wearer, meticulous attention to their care and cleaning is extremely important. If a daily-disposable lens is available in a suitable prescription, a change to this modality may be a good idea. It may be obvious, but saliva should never be substituted for lens solutions.
Makeup materials are another possible source of contamination, although it was found in a recent study that people who wear makeup are less likely to be harboring Demodex mites than others. Probably this is the result of routine nightly cleaning of the makeup from the skin and removing other debris and unwanted guests in the process. Still, replacement of all eye makeup materials each six months is highly recommended.
Summary
See an eyecare practitioner if you notice signs of inflammation in the eyelid area, because it is easy for blepharitis to become chronic if not treated.
Blepharitis causes its own symptoms, and affects other areas, such as successful contact lens wear and dry eye. It is important to follow all procedures and recommendations for treatment.
Demodex infestation is becoming more well-known by eyecare practitioners than in the past and now, more effective treatment is available.
It is important for patients to realize that no treatment currently can be considered a cure for blepharitis, and that they will need to continue with good hygiene, meticulous contact lens care and complete replacement of makeup materials every six months, to prevent re-inoculating themselves with bacteria, or allowing the return of Demodex mites.